上述的这种关联性在针对体重等因素进行分析矫正后仍然存在,更糟糕的是,患脂肪肝的抽烟者,肝纤维化、肝硬化的可能性也比不抽烟的患者要高。因此,研究人员认为吸烟是脂肪肝的独立风险因子,并且可能会促进脂肪肝恶化,强烈建议脂肪肝患者戒烟。

欧洲超市的烟盒。(摄影:史隽)
亡羊补牢
吸烟有害健康,在2019年的今天,这已经是证据充分、板上钉钉的结论了。
《新英格兰医学杂志》(NEJM)去年发表了一项研究,对超过三百万人进行了平均20年的长期随访,发现抽烟者的死亡风险远远高于不吸烟的人(不奇怪……),而戒烟者的死亡风险则比不戒烟的人要低很多[12],戒烟者死于心血管疾病的风险也大大低于抽烟者。可见,能不抽烟最好,如果已经在抽烟了,及时戒烟也还是能及时减损的(见下图)。
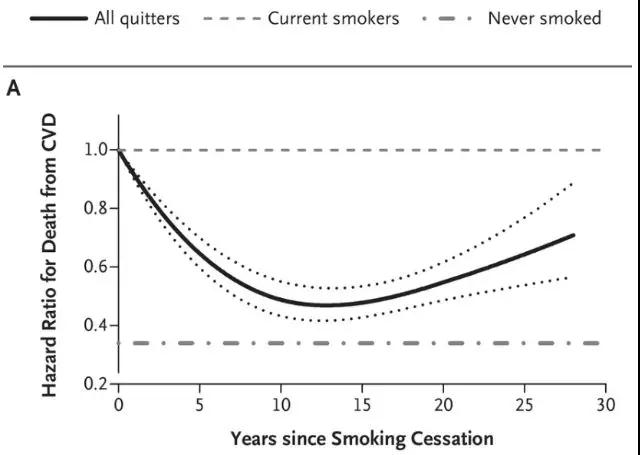
戒烟年数与心血管疾病死亡的关系,横轴为戒烟年数,纵轴为死亡率
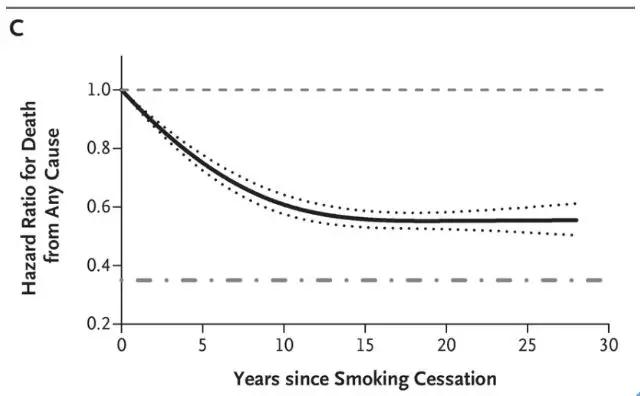
戒烟年数与全因死亡风险的关系,横轴为戒烟年数,纵轴为死亡率
前几天发表的一项关于年长女性抽烟与膀胱癌研究也得出了同一个结论:及时戒烟能及时止损[3]。
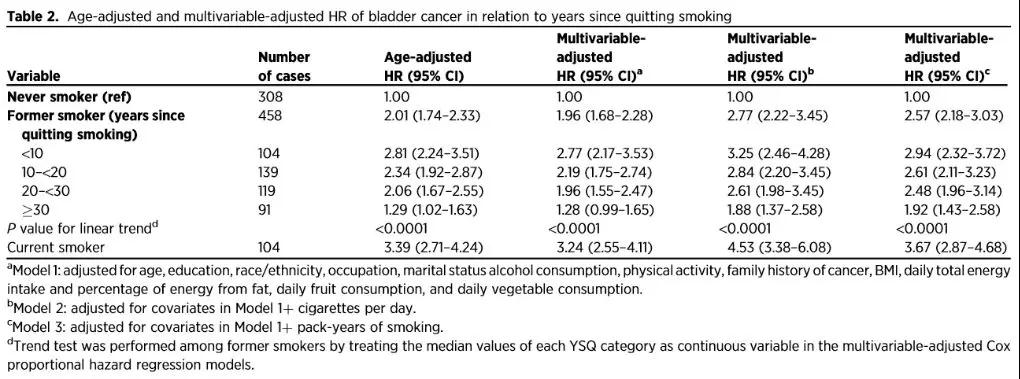
研究人员通过对143279名年龄在50-79岁的美国女性进行追踪研究,发现戒烟和抽烟的人,患膀胱癌的风险分别是从不抽烟的人的2.0倍和3.4倍,而戒烟时间越长,风险就越低。
这些数据再次说明,抽烟不好,戒烟好。而戒烟就像学习一样,什么时候开始都不晚。

作者(自我)介绍
菜菜,科学女青年,哈佛医学院讲师。
参考文献
[1] Cao, M. & Chen, W. Epidemiology of lung cancer in China. Thoracic cancer 10, 3-7, doi:10.1111/1759-7714.12916 (2019).
[2] Chen, Z. M. et al. Emerging tobacco-related cancer risks in China: A nationwide, prospective study of 0.5 million adults. Cancer 121 Suppl 17, 3097-3106, doi:10.1002/cncr.29560 (2015).
[3] Li, Y. et al. Smoking Cessation and the Risk of Bladder Cancer among Postmenopausal Women. Cancer prevention research (Philadelphia, Pa.) 12, 305-314, doi:10.1158/1940-6207.capr-18-0441 (2019).
[4] Pruss-Ustun, A. et al. Environmental risks and non-communicable diseases. BMJ (Clinical research ed.) 364, l265, doi:10.1136/bmj.l265 (2019).
[5] Byington, C. L. et al. Community Surveillance of Respiratory Viruses Among Families in the Utah Better Identification of Germs-Longitudinal Viral Epidemiology (BIG-LoVE) Study. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 61, 1217-1224, doi:10.1093/cid/civ486 (2015).
[6] Bensenor, I. M. et al. Active and passive smoking and risk of colds in women. Annals of epidemiology 11, 225-231 (2001).
[7] Zhou, G. et al. Smoking, leisure-time exercise and frequency of self-reported common cold among the general population in northeastern China: a cross-sectional study. BMC public health 18, 294, doi:10.1186/s12889-018-5203-5 (2018).
[8] Eddleston, J., Lee, R. U., Doerner, A. M., Herschbach, J. & Zuraw, B. L. Cigarette smoke decreases innate responses of epithelial cells to rhinovirus infection. American journal of respiratory cell and molecular biology 44, 118-126, doi:10.1165/rcmb.2009-0266OC (2011).
[9] Proud, D. et al. Cigarette smoke modulates expression of human rhinovirus-induced airway epithelial host defense genes. PLoS One 7, e40762, doi:10.1371/journal.pone.0040762 (2012).
[10] Mihaylova, V. T. et al. Regional Differences in Airway Epithelial Cells Reveal Tradeoff between Defense against Oxidative Stress and Defense against Rhinovirus. Cell reports 24, 3000-3007.e3003, doi:10.1016/j.celrep.2018.08.033 (2018).
[11] Jung, H. S. et al. Smoking and the Risk of Non-Alcoholic Fatty Liver Disease: A Cohort Study. The American journal of gastroenterology 114, 453-463, doi:10.1038/s41395-018-0283-5 (2019).
[12] Hu, Y. et al. Smoking Cessation, Weight Change, Type 2 Diabetes, and Mortality. The New England journal …





